Autologous Chondrocyte Implantation
Articular (hyaline) cartilage, which is composed mainly of water and a collagenous extracellular matrix, provides a smooth and resilient surface at the ends of bones, allowing virtually frictionless movement within the knee joint. It also acts as a shock absorber, cushioning the bone from forces of more than five times the body's weight. The cellular component of hyaline cartilage is the chondrocyte, which is responsible for the production and maintenance of the matrix. Cartilage lacks blood and nerve supplies, and it has a limited potential for self-repair.
 Cartilage damage in the knee can be caused directly by injury, often as a result of sporting activity, or spontaneously (a condition called osteochondritis dissecans). Softening of the kneecap cartilage (a condition called chondromalacia patellae) may be caused by trauma, overuse, parts being out of alignment, or muscle weakness, and most often occurs in young adults. Loss of cartilage alone is referred to as chondral damage, whereas loss of bone and cartilage is known as osteochondral damage. Osteochondral damage occurs more commonly in adolescents; it appears that the plane of weakness in this age group lies in the bone rather than at the junction of the cartilage and the bone. Symptoms associated with the loss of hyaline cartilage include knee pain, knee swelling, knee locking and giving way of the knee joint. Ultimately,mechanical damage to the joint surface can lead to osteoarthritis.
Cartilage damage in the knee can be caused directly by injury, often as a result of sporting activity, or spontaneously (a condition called osteochondritis dissecans). Softening of the kneecap cartilage (a condition called chondromalacia patellae) may be caused by trauma, overuse, parts being out of alignment, or muscle weakness, and most often occurs in young adults. Loss of cartilage alone is referred to as chondral damage, whereas loss of bone and cartilage is known as osteochondral damage. Osteochondral damage occurs more commonly in adolescents; it appears that the plane of weakness in this age group lies in the bone rather than at the junction of the cartilage and the bone. Symptoms associated with the loss of hyaline cartilage include knee pain, knee swelling, knee locking and giving way of the knee joint. Ultimately,mechanical damage to the joint surface can lead to osteoarthritis.
There is no uniform approach to managing hyaline cartilage defects in the knee. There are two main categories of procedures: those intended primarily to achieve symptomatic relief and those that also attempt to re-establish the articular surface. Interventions that aim to re-establish the articular surface include ACI, marrow stimulation techniques (such as abrasion arthroplasty, drilling and microfracture) and mosaicplasty (also known as osteochondral transplantation). Other treatment options include knee washout (lavage) with or without debridement.
Mosaicplasty
This technique involves removing cylinders of normal cartilage and bone (approximately 4.5 mm diameter) from 'non-weight-bearing' areas of an affected knee and placing them into areas of defective cartilage. Microfracture involves breaching the sub-chondral bone to cause bleeding, and this results in the formation of a blood clot. The clot creates the necessary conditions for a viable population of marrow stem cells to build new tissue within the lesion.
Autologous chondrocyte implantation
(ACI – formerly referred to as autologous cartilage transplantation or ACT) is an approach that has been used to treat defined, symptomatic knee cartilage defects The aim of this treatment is to enable the regeneration of hyaline or hyalinelike cartilage, thereby restoring normal joint function. ACI is not used where there is joint instability that cannot be corrected simultaneously or where there is existing osteoarthritis.
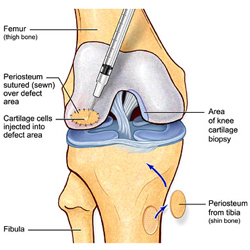
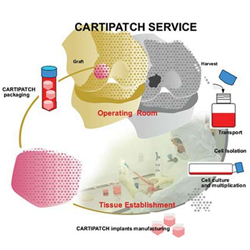
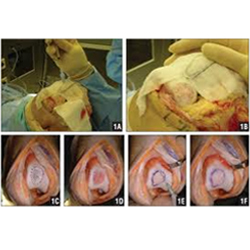
ACI comprises a series of procedures. First, chondrocytes are harvested arthroscopically from the edge of the affected knee joint. The cells are cultured for a few weeks to expand the cell population (by a factor of about 50). Then, in a second surgical procedure, the cultured chondrocytes are implanted into areas denuded of cartilage by disease or injury. Each damaged area is carefully debrided and covered with a periosteal tissue flap or a porcine collagen membrane, beneath which the autologous cells are injected. In a modification of the treatment, extracted autologous chondrocytes are cultured within a collagen matrix, which is then implanted (matrix-guided ACI). It has been argued that matrix-guided ACI has a number of advantages including allowing the second surgical procedure to be performed by a limited approach or by arthroscopic implantation. arthroscopy.
